FtM replacement Hormone Effective and Risk
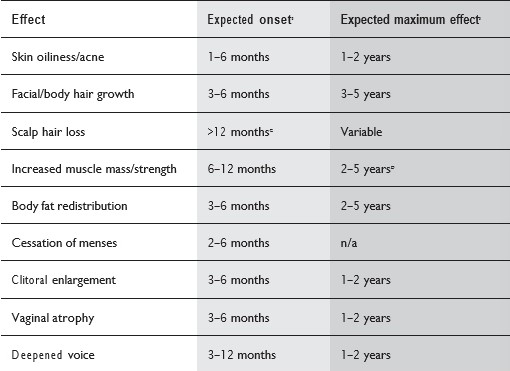
Masculinizing hormone therapy will induce physical changes that are more congruent with a patient’s gender identity In FtM patients, the following physical changes are expected to occur: deepened voice, clitoral enlargement (variable), growth in facial and body hair, cessation of menses, atrophy of breast tissue, and decreased percentage of body fat compared to muscle mass.
Most physical changes, masculinizing, occur over over years. The amount of physical change and the exact timeline of effects can be highly variable.
Table 1 shows the effect and expected time course of masculinizing hormones
Source: WPAT.Version 7 Page 37
The extent and speed of physical changes depend partly on factors like the dose, how the medication is given, and which medications are used. These choices are based on a patient's specific medical goals (like changes in how they express their gender or plans for sex reassignment) and their medical risk factors. Currently, there's no evidence that we can reliably predict how someone will respond to hormone therapy, except maybe for the deepening of the voice in female-to-male individuals. Things like age, body type, ethnicity, or family resemblance don't seem to predict how well hormone therapy will work. When everything else is the same, there's no proof that any specific type of hormone or how it's given is better at producing the changes people want.
Risks of Hormone Therapy
Every medical procedure comes with potential risks. The chance of experiencing a serious problem depends on many things, like the specific medication, how much is given, how it's given, and the patient's health situation, including age, existing conditions, family medical history, and lifestyle. So, it's hard to say for sure if a particular bad outcome will happen to a specific person.
The risks linked with masculinizing hormone therapy for transgender, transsexual, and gender-nonconforming people are sorted out in a table. These risks are grouped based on what we know into three categories: (i) risks that are likely to go up with hormone therapy, (ii) risks that might increase with hormone therapy, and (iii) risks where we're not sure or there's not enough evidence to say if there's an increased risk. Things in the last category might still be risky, but because we don't have enough evidence, we can't be certain about them.
TABLE 2: RISKS ASSOCIATED WITH HORMONE THERAPY. BOLDED ITEMS ARE CLINICALLY SIGNIFICANT
| Risk Level | Masculinizing hormones |
|---|---|
| Likely increased risk |
|
| Likely increased risk with the presence of additional risk factors | - |
| Possible increased risk |
|
| Possible increased risk with presence of additional risk factorsB |
|
| No increased risk or inconclusive |
|
Source: WPAT version 7 page 41

