Female to Male Penis Surgery
Female-to-male (FTM) gender affirmation surgery transforms the appearance of female genitalia into that of a male's. This surgery has a profound and validating effect on transgender men, enabling them to have a body that aligns with their gender identity. It allows individuals to urinate while standing, and many procedures enable them to achieve erections. The vagina is removed during the procedure, and a hysterectomy is often performed simultaneously, eliminating menstruation. There are two primary methods for creating a penis:
- Metoidioplasty: Utilizes the clitoris, which is enlarged through hormone therapy, to create a smaller penis.
- Phalloplasty: Creates a larger penis using a skin flap from the patient's forearm, thigh, or other donor site.
Individuals typically undergo hormone therapy for at least a year before either type of surgery. During phalloplasty, the surgeon also removes the vagina in a vaginectomy, and a hysterectomy is often performed at the same time.
Phalloplasty in Female-to-Male Gender Confirmation Surgery
Ideal candidates for phalloplasty meet the following criteria:
- Age: At least 20 years old. (Minors require consent from parents or legal guardians).
- Hormone Therapy: Continuous use of male hormones for at least one year.
- Gender Expression: Living and presenting as male for at least one year.
- Mental Health: Undergone a psychiatric evaluation and deemed mentally stable and fit for surgery.
- Physical Health: In good physical health.
- Prior Surgeries: Completed mastectomy and total hysterectomy-oophorectomy at least six months prior to phalloplasty.

Dr. Kamol's Experience
Since 1997, Dr. Kamol has performed over 10,000 procedures on transgender patients, including over 5,000 sex reassignment surgeries (SRS). He is recognized as one of the most experienced surgeons in gender reassignment surgery worldwide. Dr. Kamol currently performs over 500 male-to-female surgeries each year. He leads the team at Kamol Cosmetic Hospital in Bangkok, Thailand, specializing in both male-to-female and female-to-male sex transitions and facial feminization.
See more of Dr. Kamol's Profile.
Benefits of Phalloplasty
- Sexual Function: Higher likelihood of achieving penetrative intercourse.
- Phallic Size: Significantly larger phallus compared to metoidioplasty.
- Appearance: Creates more natural-looking penis.
Phalloplasty Techniques at Kamol Cosmetic Hospital
Kamol Cosmetic Hospital offers several phalloplasty techniques:
1. Anterolateral Thigh Pedicle Flap (ALT-Phalloplasty)
This is the preferred technique at Kamol Hospital. It utilizes skin, along with its underlying nerves and blood vessels, from the front and outer thigh to construct the penis. Due to individual variations in patient needs and preferences, Kamol Hospital offers different surgical options for ALT-phalloplasty:
- Full Phalloplasty with Urethral Lengthening: A two-stage procedure involving urethral prefabrication and total vaginectomy at least 6 months before the ALT flap phalloplasty. This allows for urination through the neophallus (new penis). The urethra and sensory nerves are connected during the surgery.
- Phalloplasty with Metoidioplasty: Combines a previously performed metoidioplasty with ALT-phalloplasty. The ALT flap is placed on top of the existing micropenis, and the sensory nerves are shared. Urination is possible through the micropenis. This technique avoids potential urethral complications like strictures or fistulas.
- Phalloplasty without Urethral Lengthening: A simpler procedure without urethral reconstruction. Urination occurs through the original urethra. The surgical scar is located at the base of the penis. This is a non-vessel anastomosis technique, thus minimizing the risks of vascular thrombosis.
ALT-Phalloplasty Donor Site Preparation
- Hair Removal: Hair removal from the front and side of the thighs is necessary to prevent hair growth on the neophallus.
- Skin Thickness: Thin thigh skin is ideal. Skinfold thickness at the mid-front thigh should be less than 1.5 cm. Patients with thicker skin may require weight loss, exercise, or liposuction before surgery.
- Donor Site Coverage: The donor site on the thigh is covered with a split-thickness skin graft from the adjacent area.
- Pre-expansion: For patients who want to avoid a skin graft, pre-expanded ALT-phalloplasty with tissue expansion is an option. This requires the patient to stay 1-2 months for thigh skin expansion before the flap surgery.
- Prior Surgeries: Vaginectomy, hysterectomy, and oophorectomy should be completed at least 6 months before penile reconstruction.
References
- van der Sluis WB., Ronkes BL., Steensma TD., Al-Tamimi M., van Moorselaar., Bouman BM., Pigot Garry LS. Comparison of surgical outcomes and urinary functioning after phalloplasty with versus without urethral lengthening in transgender men. Int J Trans health. https://doi.org/10.1080/26895269.2022.2110548
- Colebunders SD., Stillaert F., Monstrey S. Pre-expanded Anterolateral Thigh Perforator Flap for Phalloplasty. Clin Plast Surg. 44(1):129-141. https://doi.org/10.1016/j.cps.2016.08.004
Advantages of ALT Phalloplasty
- Good skin color match.
- Larger girth compared to RFF phalloplasty.
- Some natural rigidity.
- The less noticeable donor site, is easily concealed with clothing.
- Reduced surgical time with pedicled ALT.
- Good sensation.
- Good potential for urethroplasty.
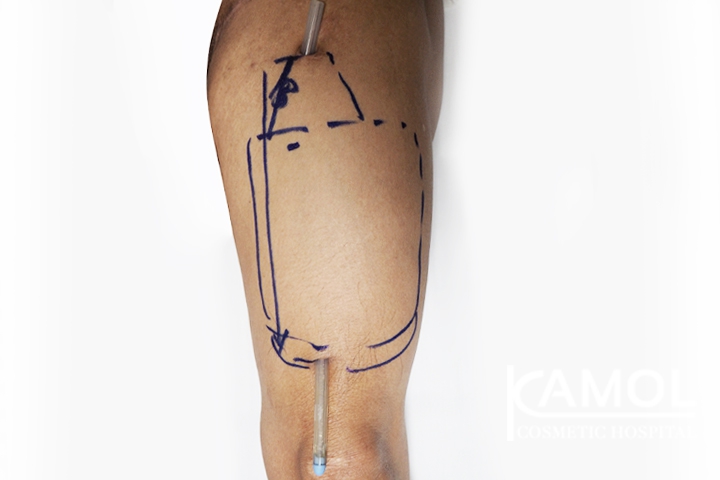
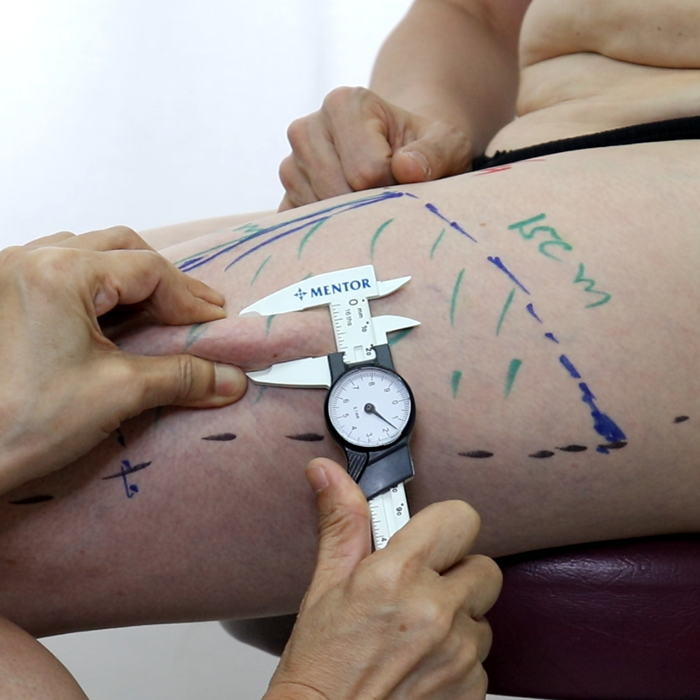
How to Prepare the ALT Donor Site
- Mark the site on the non-dominant thigh (15x18 cm), as shown in the video clip.
- Remove hair from the marked area.
- Check skin quality and ensure the skin pinch is less than 1.5-1.8 cm. Liposuction may be necessary for thicker skin, followed by a waiting period of 6 months to a year to allow the skin to soften.
- If the patient needs urethral prefabrication, it can be done a few months after liposuction.
- Phalloplasty can be performed after preparing the donor site.
- A penile implant can be considered 1-2 years after phalloplasty.
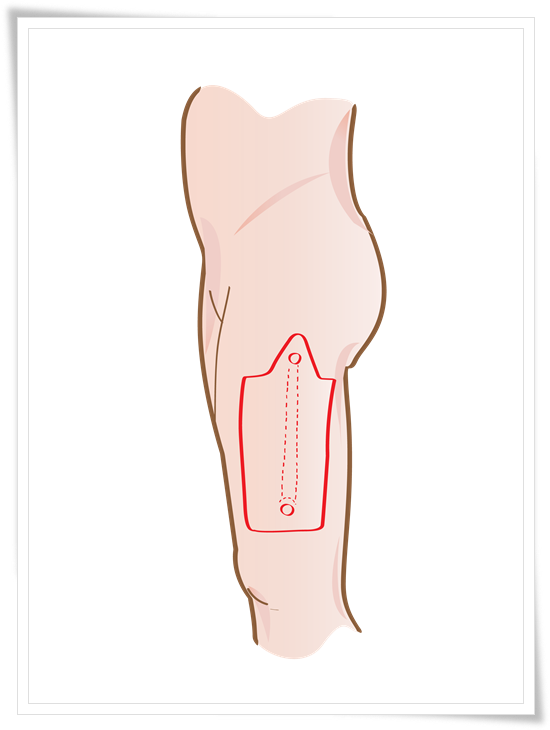
Picture 1: ALT-Pedicle Flap
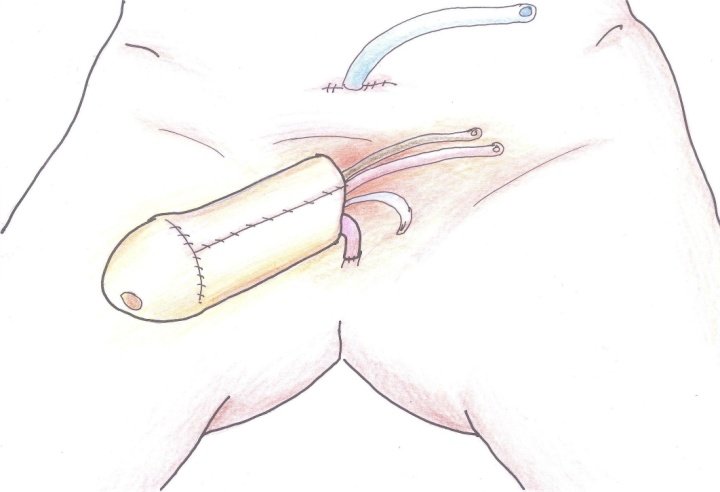
Picture 2:ALT phalloplasty creation
How to prepare the ALT donor site?
1. Mark the site at the nondominant Thigh 15x18 cm as shown in the video clip
2. Hair Removal in this area
3. Check the skin's quality and ensure the skin pinch is less than 1.5-1.8 cm. In case of over-thickness, the patient can do liposuction and then wait for 6 months to one year to make the skin softer. We can create phalloplasty. If the patients need to do urethral prefabrication, they can do it a few months after liposuction. If the patient does not need urethral with phalloplasty, they can do phalloplasty after preparing the donor site. After 1-2 years after phalloplasty, they can do the implant
 |
 |
 |
| Donor site | Skin Pinch | Urethral Preflabriation |
Picture 3: How to prepare the ALT donor site
ALT Phalloplasty Without Urethral Integration
This variation of phalloplasty creates a neophallus without integrating a urethra. Individuals who undergo this procedure will not be able to urinate through the neophallus and will require alternative methods like a urinary catheter. This type of phalloplasty is typically recommended for individuals who have medical conditions that make it difficult to connect the urethra to the neophallus or for those who are not interested in undergoing urethral integration. The ALT Phalloplasty Without Urethral Integration procedure typically involves the following steps:
- Anesthesia: Before the procedure, the patient is given general anesthesia to ensure they are completely unconscious and pain-free during the surgery.
- Donor Site Selection: The surgeon will select a donor site for the tissue that will be used to construct the neophallus. This can be taken from the patient's own body (autograft) or a donated source (allograft).
- Tissue Harvesting: The selected tissue is harvested and prepared for constructing the neophallus.
- Neophallus Creation: The surgeon will then use the harvested tissue to construct the neophallus, taking care to shape it in a manner that resembles a natural penis.
- Closure: After the neophallus has been constructed, the incisions are closed, and the patient is moved to the recovery room.
Benefits of ALT Phalloplasty Without Urethral Integration
- Improved Aesthetic Appearance: The neophallus constructed during this procedure can be shaped to resemble a natural penis, thus enhancing the individual's overall appearance and increasing their confidence.
- Lower Risk of Complications: By avoiding the integration of the urethra, there is a lower risk of complications such as urethral strictures or fistulas.
- Shorter Recovery Time: The absence of urethral integration typically means a shorter recovery time, allowing the patient to return to normal activities more quickly.
Conclusion: ALT Phalloplasty Without Urethral Integration is a variation of the standard phalloplasty procedure that involves creating a neophallus without integrating a urethra. This procedure is recommended for individuals with medical conditions that make it difficult to connect the urethra to the neophallus or for those who are not interested in undergoing urethral integration.
2. Alternative Phalloplasty Options at Kamol Cosmetic Hospital
2.1 Radial Forearm Free Flap (RFF)
This technique uses skin from the front of the forearm to create the neophallus. It involves microsurgery to connect the blood vessels and nerves of the forearm skin flap to the groin area.
RFF Techniques:
- Two-Stage Technique: Urethral prefabrication is performed six months before the main phalloplasty. Suitable for patients with smaller forearms.
- One-Stage Technique: Neophallus and neourethra are constructed simultaneously in a single surgery.
Advantages of RFF:
- Thinner skin in the forearm area, which can be advantageous for creating a more aesthetically pleasing neophallus.
Disadvantages of RFF:
- Donor site scar can be difficult to conceal, potentially impacting self-consciousness and clothing choices.
- There is a risk of partial skin graft loss, which may necessitate further procedures or revisions.
- Decreased sensitivity in the neophallus can affect sexual function and pleasure.
- Possible hand motion issues due to the removal of skin and tissue from the forearm.
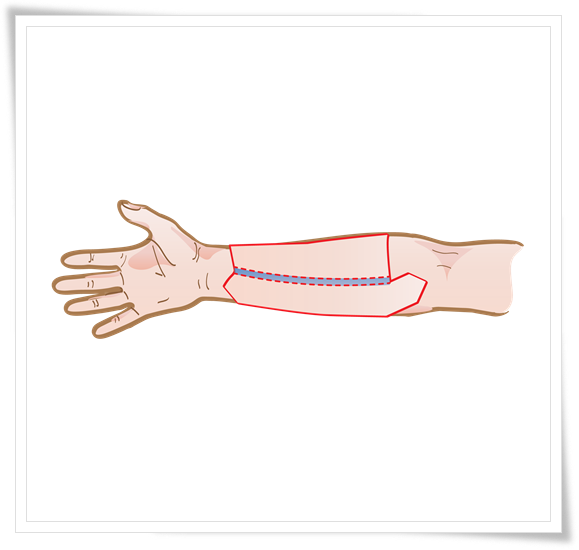
Picture 4: Radial Forearm Free Flap
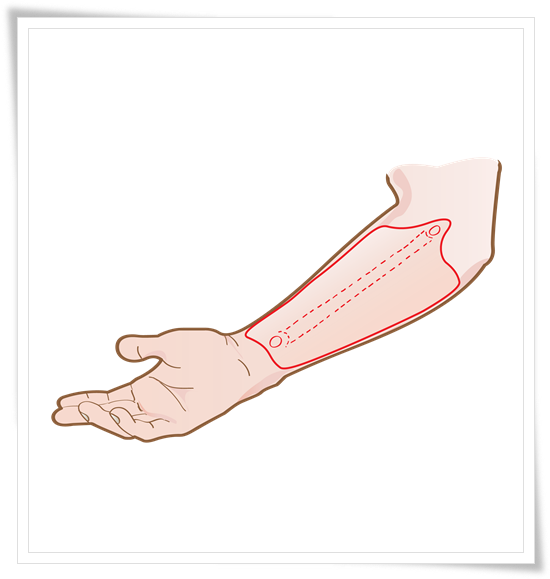
Picture 5: Radial Forearm Free Flap
2.2 Fibula Free Flap (FFF)
This technique utilizes skin, nerves, and a portion of the fibula bone (from the lower leg) to construct the neophallus. Microsurgery is used to connect the blood vessels and nerves.
FFF Technique:
- A one-stage procedure where the neophallus is created using the fibula bone, skin, and nerves. The neourethra is pre-laminated in situ for six months before the main surgery.
Advantages of FFF:
- The flap has a long and reliable blood supply, reducing the risk of complications.
- Less prominent scarring at the donor site compared to other techniques.
- The use of the fibula bone provides natural rigidity for penetration.
Disadvantages of FFF:
- The phallus may have a more rigid appearance, which may not be aesthetically desirable for all individuals.
- There is a potential for bone resorption over time, which could affect the size and shape of the neophallus.
- Potential curving and fracture of the autologous bone transplants can occur, requiring further intervention.
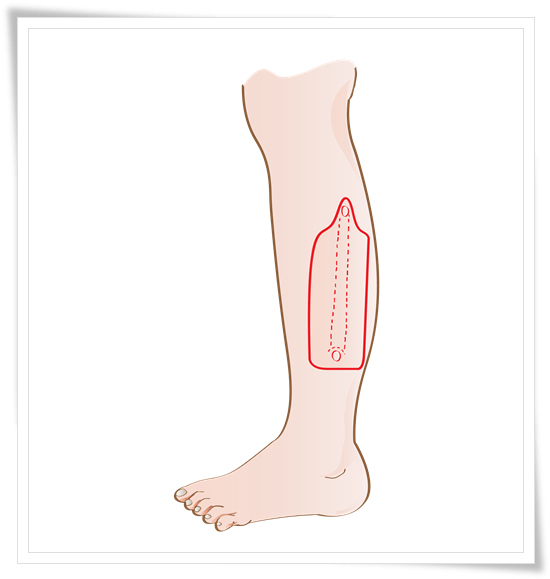
Picture 6: Fibula Free Flap
2.3 Musculocutaneous Latissimus Dorsi (MLD) Flap
This technique uses a skin flap with nerves and blood vessels from the back (latissimus dorsi muscle) to create the neophallus. Microsurgery connects the flap to the groin area.
MLD Technique:
- A two-stage procedure. The first stage involves transferring the skin flap to the genital area. The second stage involves constructing the neourethra.
Advantages of MLD:
- The donor site is less conspicuous, making it easier to conceal scarring.
- The donor site is relatively hairless, reducing the risk of hair growth on the neophallus.
- This technique can provide good aesthetic outcomes, resulting in a natural-looking neophallus.
- There are possibilities for penetrative sex with this technique.
Disadvantages of MLD:
- The phallus may have poor sensitivity, affecting sexual function and pleasure.
- The phallus can be large, potentially requiring additional debulking procedures to achieve the desired size and shape.
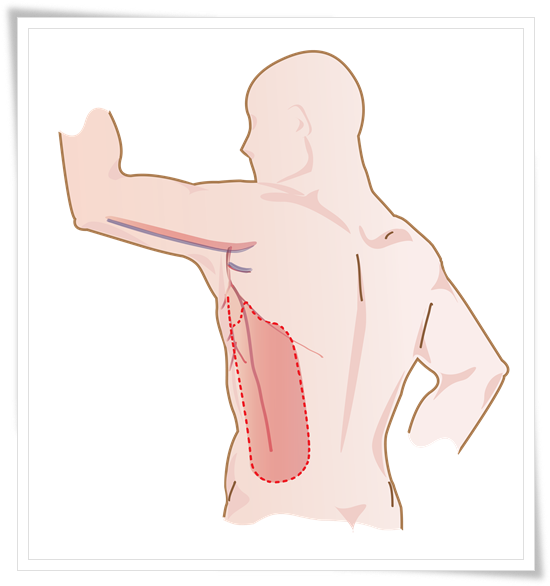
Picture 7: Musculocutaneous Latissimus Gorsi (MLD)
Urethral Reconstruction in Phalloplasty
Kamol Cosmetic Hospital currently offers three options for neourethral reconstruction:
- Skin graft from the groin: This involves taking a skin graft from the groin area to create the lining of the new urethra.
- Peritoneum: The peritoneum, a thin membrane that lines the abdominal cavity, can be used to create the urethra.
- SCIP flap (Superiorly based Circumflex Iliac Artery Perforator flap): This involves using a flap of skin and tissue from the lower abdomen to create the urethra.
Comparison of different Phalloplasty techniques
| Flap technique | Size of neo penis | Donor scar | Sensation | Self-stiffness |
|---|---|---|---|---|
| ALT | Medium-to-Large | Thigh | Yes | No |
| MLD | Medium-to-Large | Side of Torso | Yes | No |
| Radial forearm | Small -to-medium | Forearm | Yes | No |
| Fibula | Small | Leg | Yes | No |
Preparing for Phalloplasty
- Consultation with the surgeon: This is crucial to discuss your surgical goals, medical conditions, and any current treatments you are undergoing. The surgeon will assess your suitability for the procedure and explain the different techniques available.
- Stop smoking and drinking alcohol: It is essential to stop smoking and avoid alcohol for at least 2 weeks before surgery to promote healing and reduce the risk of complications.
- Stop certain medications, vitamins, or herbs: You will need to stop taking any medications, vitamins, or herbs that interfere with blood clotting, such as aspirin, as advised by your surgeon.
Phalloplasty Techniques and Considerations
Several techniques can be used to perform a phalloplasty, and the choice of technique depends on the patient's specific needs and goals. Some of the more common techniques include the radial forearm phalloplasty, the anterolateral thigh phalloplasty, and the free flap phalloplasty. Like any surgical procedure, phalloplasty carries certain risks and complications. These can include infection, bleeding, scarring, and problems with the skin flaps used to construct the penis. In addition, there is a risk of damage to the nerves and blood vessels in the area, which can result in decreased sensitivity or impaired blood flow. After a phalloplasty procedure, it is important for the patient to follow their surgeon's postoperative care instructions carefully in order to minimize the risk of complications and optimize the healing process. This may include taking medications as prescribed, keeping the incision site clean and dry, and avoiding strenuous activities. In some cases, physical therapy may be recommended to help improve the function of the newly constructed penis.
Risks and Complications for Phalloplasty
- Infection: As with any surgery, there is a risk of infection following a phalloplasty procedure. This can be serious and may require additional treatment, such as antibiotics.
- Bleeding: There is also a risk of bleeding during or after the surgery. This may sometimes require a return to the operating room to control the bleeding.
- Scarring: Scarring is a common complication of phalloplasty. The extent of scarring will depend on the specific technique used and the patient's healing process.
- Problems with skin flaps: The skin flaps used to construct the penis during a phalloplasty procedure may not heal properly or may not have a satisfactory appearance. In some cases, additional surgery may be needed to correct these issues.
- Nerve and blood vessel damage: During a phalloplasty procedure, there is a risk of damage to the nerves and blood vessels in the area. This can result in decreased sensitivity or impaired blood flow to the newly constructed penis.
- Failure to achieve desired results: Patients should have realistic expectations about the outcome of a phalloplasty procedure. In some cases, the results may not be as expected, and additional surgery may be needed to achieve the desired outcome.
Getting to Know for Phalloplasty Surgery
How to prepare for phalloplasty donor site
Preparing for phalloplasty donor site surgery is an important step in ensuring a successful procedure and a smooth recovery.
How to detransition from MTF to Male?
Detransitioning is the process of reversing a gender transition. In the case of MtF detransitioning, individuals who have undergone
Comparision between ALT and MLD phalloplasty
There are several techniques available for phalloplasty, including Anterolateral Thigh (ALT) Phalloplasty and Musculocutaneous Latissimus Dorsi (MLT) Flap Phalloplasty.
Reviews for ALT Phalloplasty
Video : Testimonials of Phalloplasty
Why is Kamol Cosmetic Hospital famous for Phalloplasty?
Kamol Hospital is a popular choice for phalloplasty surgery for several reasons, including its expertise and experience, state-of-the-art facilities, comprehensive pre and post-operative care, patient-centered approach, and reputation for excellence in gender affirmation surgeries.
Expertise and Experience:
One of the critical reasons Kamol Hospital is famous for phalloplasty surgery is the expertise and experience of its surgical team. The hospital has a team of highly skilled and experienced surgeons who specialize in gender affirmation surgeries, including phalloplasty. They have performed numerous successful surgeries, and their expertise in this field is widely recognized.
State-of-the-art Facilities:
Another factor that makes Kamol Hospital popular for phalloplasty surgery is its state-of-the-art facilities. The hospital is equipped with modern and advanced surgical equipment and facilities that ensure the highest safety and quality of patient care. The hospital also has advanced imaging technology for surgical planning and patient education.
Comprehensive Pre- and Post-operative Care:
Kamol Hospital provides comprehensive pre and post-operative care to ensure patients receive the best possible outcome and experience. Before surgery, patients undergo a thorough medical evaluation and counseling to ensure they are physically and mentally prepared for it. After surgery, patients receive follow-up care, including counseling and support services, to aid in their recovery.
Patient-Centered Approach:
Kamol Hospital takes a patient-centered approach to care. This means that they work closely with patients to understand their individual needs and preferences and tailor the treatment plan accordingly. The hospital's staff is highly trained to provide compassionate care, prioritizing patient comfort and satisfaction throughout treatment.
Reputation:
Kamol Hospital has built a reputation for excellence in gender affirmation surgeries, including phalloplasty. Many patients undergoing surgery at Kamol Hospital have shared positive feedback and experiences, contributing to its popularity. The hospital's commitment to patient-centered care, state-of-the-art facilities, and experienced surgical team have earned it a reputation as a top choice for phalloplasty surgery.
Why Thailand is a plastic surgery destination?
Thailand is a top destination for plastic and cosmetic surgery. The high quality and specialist skills of the surgeons, the first-class hospital treatments, and the affordable cost all add up to a satisfying all-around package. There is also the added temptation to recover post-procedure in luxury hotels or recovery service apartments.
Frequently Asked Questions (FAQs)
A: Phalloplasty is a surgical procedure used to construct a neophallus (new penis) for transgender men or individuals with certain medical conditions. It's a key component of female-to-male (FTM) bottom surgery, which aims to create male-typical genitalia.
A: Several techniques are used in creating a new penis, each with its own advantages and disadvantages:
- Anterolateral Thigh Flap (ALT): This is the most common technique, using skin and tissue from the thigh. It offers a good skin color match, the potential for sensation, and a less noticeable donor site.
- Radial Forearm Free Flap (RFF): Uses skin from the forearm. It provides thinner skin, but the donor site scar can be more visible.
- Fibula Free Flap (FFF): Employs skin, nerves, and a portion of the fibula bone (lower leg). It offers natural rigidity due to the bone graft but may have a less natural appearance.
- Musculocutaneous Latissimus Dorsi Flap (MLD): Uses skin and muscle from the back. It provides a less conspicuous donor site but may result in a larger phallus requiring further refinement.
A: The procedure offers several benefits:
- Improved Body Image and Self-Esteem: Aligns the body with gender identity, thus leading to increased confidence and self-acceptance.
- Sexual Function: Enables standing urination and, with certain techniques, the potential for penetrative intercourse.
- Appearance: Creates more natural-looking male genitalia.
A: As with any surgery, the procedure carries potential risks:
- Infection
- Bleeding
- Skin Flap Problems: May include partial or complete flap loss, requiring revision surgery.
- Urethral Complications: Strictures, fistulas, or difficulty urinating.
- Nerve Damage: This can lead to numbness or decreased sensation in the neophallus.
- Scarring
- Unsatisfactory Aesthetic Outcome
A: Generally, good candidates for the procedure:
- Are over 20 years old (or have parental consent if younger).
- Have been on hormone therapy for at least one year.
- Have lived as a male for at least one year.
- Are in good physical and mental health.
- Have realistic expectations about the surgery's outcome.
A: The procedure creates a neophallus (new penis) that resembles a penis in appearance and allows for standing urination. However, achieving full sexual function, including erections and orgasms, often requires additional procedures like penile implants.
A: Urethral reconstruction is a crucial part of creating a new penis. It involves creating a new urethra within the neophallus, allowing for urination through the penis. Different techniques can be used, including skin grafts or flaps from various donor sites.
A:
- One-stage: The neophallus and urethra are constructed in a single operation.
- Two-stage: Often involves creating the urethra first (urethral prefabrication) and then constructing the neophallus in a separate surgery, at a later date.
A: A penile implant is a medical device surgically placed inside the penis to help achieve erections. It's typically considered after the initial phalloplasty has healed, often 1-2 years later.
A: Recovery varies depending on the specific technique used. It typically involves:
- Hospital Stay: A few days to a week.
- Pain Management: Medications to manage discomfort.
- Wound Care: Keeping the incisions clean and dry to prevent infection.
- Activity Restrictions: Avoid strenuous activity and heavy lifting for several weeks.
- Compression Garments: May be used to help reduce swelling.
- Follow-up Appointments: Regular check-ups with the surgeon to monitor healing.
A: The results of female-to-male penis surgery are generally permanent. While refinements or revisions may be needed in some cases, most individuals experience significant improvement in body image, self-esteem, and quality of life.
A: The total cost of phalloplasty can vary significantly, depending on the required surgical technique, your surgeon's fees, the relevant hospital charges, and your geographical location.
Rest assured your surgeon can provide you with a detailed breakdown of the costs involved during the consultation phase.
A: Insurance coverage for phalloplasty varies. Some insurance plans may indeed cover female-to-male penis surgery as part of gender-affirming care, while others may not.
We advise you to check with your insurance provider to understand your coverage before making any final commitments.
A: Choosing a qualified and experienced surgeon is crucial. Consider the following:
- Board Certification: Make sure your chosen surgeon is board-certified in plastic surgery or a related field.
- Experience: Look for a surgeon with extensive experience in phalloplasty and FTM bottom surgery.
- Reviews and Testimonials: Look at before and after photos of previous procedures, read plenty of reviews and testimonials from previous patients.
- Communication: Choose a surgeon who listens to your concerns and answers your questions clearly.
A: Some important questions to ask during female-to-male penis surgery consultation:
- What techniques do you specialize in?
- What are the potential risks and complications specific to my case?
- What are the realistic expectations for the outcome?
- What is the estimated recovery time?
- What are the costs involved?
- Can I see before-and-after photos of your previous patients?
Asking these questions and having an open discussion with your surgeon will empower you to make an informed decision about whether phalloplasty is indeed right for you, and choose the best approach for your individual needs and goals.