Bariatric Surgery in Bangkok, Thailand
Modern lifestyle can be complicated, especially when it comes to eating right and living healthily. More and more we are faced with genetically modified food or fast food with inadequate nutrition and a busy, hectic lifestyle with not enough exercise. The problems that follow, among many health issues, are obesity such as diabetes, hypertension, coronary heart disease, and high cholesterol.
BMI or body mass index is an indication of obesity, calculated from weight and height in order to determine the balance between weight to height. BMI can be calculated by the body weight (kg) divided by the square of their height (m), the results can be interpreted as follows.
- Underweight: less than 18.5 (<18.5).
- Ideal: greater than or equal to 18.5 but less than 25 (≥18.5 but <25).
- Overweight: greater than or equal to 25 but less than 30 (≥25 but <30).
- Obese: greater than or equal to 30 but less than 40 (≥30 but <40).
- Risk: greater than or equal to 40 (≥40).
(https://en.wikipedia.org/wiki/Body_mass_index)
Guidelines to treat obesity
1. Diet plans and exercise
2. Treatment with medication
3. Treat with medicine
4. Surgery
Diet plans and exercise
To safely and effectively treat obesity, healthy, low-carb and low-sugar diet should be incorporated in the patient’s lifestyle along with exercise sessions no less than 4 times a week. To achieve desirable result, each exercise session should also include at least 30 minutes of cardio workout, i.e. running, cycling or swimming, as it helps burn fat. If your BMI is higher than 30 and you have risk factors, please consult with your doctor.
Treatment with medication
For those with BMI of 30 or higher, treatment with medication can be administered with close supervision of a specialist doctor. This treatment plan is also suitable for those with 27 or higher BMI with risk factors involved.
Bariatric Surgery
1. Gastric Sleeve (Sleeve Gastrectomy)
Procedure:
Today sleeve gastrectomy is the fastest-growing weight-loss surgery option in North America and Asia. In many cases, but not all, sleeve gastrectomy is as effective as gastric bypass surgery, including weight-independent benefits on glucose homeostasis. The precise mechanism(s) that produce these benefits is however not known.
(https://en.wikipedia.org/wiki/Gastric_bypass_surgery)
Advantages: This is the best way to lose weight. Diabetes, heart disease, high blood pressure and high blood cholesterol could also be cured with this procedure.
Disadvantages: Calcium, iron and vitamin deficiency might occur. There is a risk of bone erosion and anemia.
At Kamol Cosmetic Hospital, we use the minimal invasive surgery or laparoscopy which only causes small lesions on the abdomen.
Picture 1. Shows Vertical Sleeve Gastrectomy
http://www.nuffieldhealth.com/treatments/sleeve-gastrectomy
Preparations for Bariatric Surgery
A list of specialists to consult with before the surgery
1. Nutritionists
They can set up new diet plans and determine how much food should the patient consume after surgery, and how to lose weight before surgery.
2. Psychologists
Help manage and reduce stress before and after surgery.
3. Physicians specializing in obesity
Doctors of medicine closely monitor health conditions of the patient. They may offer counseling or medication for weight loss before the surgery.
4. Expert surgeons doing surgeries on obese patients
Surgery can be performed in specific cases. However, there are advantages and disadvantages to this surgery and the patient has rights to inquire before deciding to receive the surgery.
For consultation and practice
- The nutritional therapy to explain how much client should eat after surgery. And how to lose weight before surgery.
- Psychologists help in reducing the stress that may be more in the before - after surgery.
- Doctors of Medicine need to monitor health counseling therapy. Counseling or medication to lose some weight before the surgery.
- Medical-surgical alternative for patients that describes the procedures for each type has its advantages. The downside, however, the patient will be considered to have any right to them.
Complications:
- Bleeding
- Infections
- Outflow tract (tears in the bowels
- Follow-up or corrective surgeries
Postoperative complications may include blood clots from pulmonary disease, pneumonia or urinary tract infection, which are similar to any surgery. However, complications may occur less if the surgery is performed in a hospital or a medical center with team of expert doctors, especially anesthesiologists with expertise in handling obese patients. Post-surgery, proper equipment and care must be provided to monitor the patient, including teams of nurses and specially trained caregivers.
Why is weight loss surgery good?
With less weight and obesity, a person has lower health risks that include diabetes, hypertension, heart disease, cancer, sleep apnea among many others. Also, people with less obesity requires less expenses to care for their health
What happens after the surgery?
- Patients must be admitted in a hospital for three days to make sure that there are no complications and can function without taking analgesic.
- Exercise as soon as they feel better with exercise program designed specifically for them.
- Adopt new diet plan designed by nutritionist for at least one month.
2. Gastric Balloon
The gastric balloon is an effective solution to severe obesity. It is recommended for patients that need to lose weight before having a weight-loss operation to reduce their surgical risk.
A deflated balloon is placed through the mouth and esophagus, then filled with liquid, which is designed to partially fill your stomach, giving you a feeling of fullness. This will help you change your eating pattern, reduce the volume of food eaten and making you feel full quicker. The balloon is designed to stay in place for a maximum of six months, after which it must be removed in a similar way it was inserted.
How is the balloon inserted?
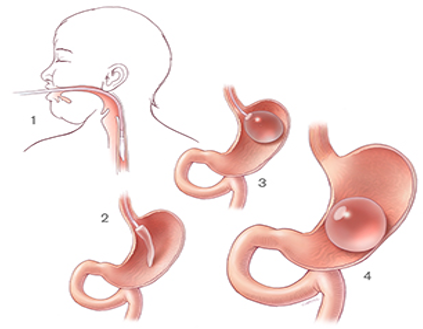
Picture 2. Shows Gastric Balloon procedures
(Ref: www.loyolamedicine.org/weight-loss-bariatrics/gastric-balloon)
In the treatment room, your throat will be sprayed with a numbing spray. It tastes unpleasant but it is very effective and within a few seconds, your throat will feel numb. Although this is quite a strange feeling, it is harmless and will help you tolerate the gastroscopy tube (camera). If you have false teeth, you will need to remove them. You may also be able to have an injection to make you feel sleepy if you wish, but this will be discussed with you.
Once the nurse has made you comfortable on the trolley, a plastic mouth guard will be put between your teeth and gums to keep your mouth slightly open. Throughout the procedure your pulse, blood pressure, breathing, and oxygen levels will be monitored, and a small sponge may be placed into one nostril to provide you with a little oxygen. This is completely routine and there is nothing to worry about.
An endoscope will then be passed through your mouth and down into your stomach. This will not cause you any pain and will not interfere with your breathing. In order to have a clear view of your stomach, it may be necessary to put some air down the endoscope. This may give you the feeling of wanting to belch. Once the endoscope has been removed, the surgeon will pass the deflated balloon through your mouth and down into your stomach. The endoscope will be reintroduced to check that the balloon is in the right position before inflating it with liquid.
Pre-procedure diet for Gastric Balloon
Before insertion of the gastric balloon, you must fast from food and drinks for 12 hours. When the gastric balloon is to be removed, you must start on a fluid-only diet 48 hours beforehand. This means no solid food at all. At this point, it may be helpful to have some fizzy drinks, as they can help cleanse the balloon, making it easier to remove. You must fast 12 hours before the balloon is due to be removed. This means no food or drinks.
What diet will I follow once I have had the balloon inserted?
For the first week, you will need to follow a fluid-only diet. This allows the stomach to get used to the balloon. You need to drink plenty of fluid to prevent dehydration.
The key points are:
• Drink slowly, sip at drinks
• Do not drink more than 100ml at once
• Drink about 2 liters (8 cups) a day.
The best fluids are low-fat or low-sugar varieties. These include semi-skimmed or skimmed milk, low-fat yogurt drinks, and soup with no lumps. Coffee and fizzy drinks must be avoided.
Over the following week, you will progress onto a pureed diet, followed by a soft, mushy diet, building up finally to a normal diet. You will see the dietitian one week after the balloon insertion to discuss the stages. Also, your long-term plan will be discussed at this appointment.
If you suffer from diabetes, you may need to monitor and record your blood sugar levels very closely, as a change in your medication may be required.
What are the benefits of having a Gastric Balloon?
Having a gastric balloon helps you to achieve short-term weight loss. It also helps to reduce health-related problems such as:
• Diabetes
• High blood pressure
• Heart disease
• Joint pain
• High cholesterol
Risks and Complications for Gastric Balloon
Most people have a few problems during and after the procedure. However, sometimes there may be complications or difficulties, such as:
• Bleeding or perforation due to injury during insertion or removal of the balloon, requiring surgical correction.
• Low blood oxygen levels or irregular heartbeat (occasionally, this is serious enough to cause a heart attack). Your oxygen level and pulse will be monitored throughout the procedure so that we can watch out for these problems.
• There is a slight risk to crowned teeth or bridgework. The risk can be reduced by telling us if you have either of these.
• Bowel blockage by the balloon, when a partially deflated balloon passes into the small bowel. This is extremely rare, but if it occurs, it needs to be removed during an operation or an endoscopic procedure.
• A blue dye is added to the saline injected into the balloon so that in the rare event that the balloon was to leak, you would know immediately by the change in color of your urine. If this happens, you should contact the hospital immediately so the balloon can be safely removed.
• Stomach discomfort, nausea, and vomiting are common for the first week following the balloon placement, but this rarely continues after this time.
• Feeling of heaviness in the abdomen or abdominal or back pain
• Acid reflux and indigestion (you will be prescribed medication to reduce your stomach acid production while the balloon is in place)
• Very rarely do patients develop a chest infection after the procedure. If you develop a cough, contact your doctor.
The chance of these risks occurring is small, but it is important that you are aware of them and that you have all the information you need before agreeing to the procedure.
What happens before the procedure?
If the gastric balloon procedure is safe and suitable for you, you will be asked to attend the hospital for a pre-procedure assessment. At this appointment, we will ask you questions about your medical history, medication, and any other operations you may have had. You may need to undergo some routine tests, such as a heart trace (ECG), X-ray, and blood tests.
What happens on admission to the hospital?
You will come to the hospital on the morning of your procedure unless told otherwise. On admission, the doctors and nurses will answer any further questions you may have. A nurse will check that there have been no significant changes in your health since your pre-assessment, and your temperature, pulse, blood pressure, and breathing will all be recorded. Before your procedure, you will be asked to wear a gown. You will also be asked to wear compression stockings (anti-embolic). They help blood flow in the deep veins in the legs, reducing the risk of developing blood clots. You will need to wear these for approximately six weeks after your procedure. You will be asked to walk to the procedure room.
Will I be put to sleep?
A numbing throat spray will be used before the procedure. Alternatively, medication may be given through a tube in your arm or hand, making you sleepy. You should still be able to hear what is being said and cooperate with verbal instructions, but later, you may have little or no recall of the procedure.
What can I expect after the procedure?
From the procedure room, you will be transferred to the ward. The nursing staff will check your pulse, blood pressure, temperature, and breathing. You may have a sore throat as a result of the endoscopic equipment. If you have had some sedation, you may feel sleepy for a while, and you may be given oxygen through two little prongs in your nose until you are fully awake. You will be encouraged to get up and move around soon after your procedure. This is to reduce the risk of developing a blood clot.
Will I feel sick?
Many people feel sick and vomit after the procedure and for some time afterward. You will be prescribed anti-sickness medication, which are drugs to help relieve the nausea and vomiting. The sickness should settle once your stomach has become used to the presence of the balloon.
Will I be in pain?
You may feel heaviness in your abdomen and pain in your abdomen and back. You will be prescribed painkillers to help relieve this.
When will I be able to go home?
Depending on how you feel, you can usually go home on the day of or the day after your procedure. However, you must have someone responsible to take you home because you may still be feeling the effects of sedation. We also advise that someone stay with you for 24 hours.
What will follow-up care be?
Approximately one week after going home, you will be sent an appointment to see the outpatient department's dietitian and nurse specialist. You will also be given the phone numbers of the specialist nurse and dietitian to contact for any advice you may need at other times. Six months after insertion, when your balloon is ready to be removed, the hospital will make arrangements and send you an appointment.
- Ref: Doncaster and Bassetlaw Hospitals NHS Foundation Trust. (2012). Gastric Balloon procedures. Bariatric surgery
Getting to Know for Bariatric Surgery:
Sleeve gastrectomy diet
Sleeve gastrectomy is a type of weight loss surgery that involves reducing the size of the stomach,...
Sleeve gastrectomy vs Gastric bypass
Obesity is a growing problem worldwide and bariatric surgery has become an increasingly popular...
What are the side effect of sleeve gastrectomy?
It is important to understand that like any other surgery, it is associated with certain risks and complications.
See more
Reviews for Sleeve Gastrectomy
Why is sleeve gastrectomy considered for weight loss?
Sleeve gastrectomy, also known as a vertical sleeve gastrectomy, is a weight loss surgery that involves removing a large portion of the stomach, leaving a smaller "sleeve" shaped stomach. This smaller stomach can hold less food, so patients feel full more quickly and eat less. The procedure is typically performed laparoscopically, which is less invasive than open surgery and has a faster recovery time.
One key benefit of sleeve gastrectomy is that it can lead to significant weight loss. On average, patients can expect to lose 50-70% of their excess weight within the first year after surgery. Weight loss is also more stable and long-lasting than other weight loss options such as diet and exercise.
Sleeve gastrectomy also leads to hormonal changes that promote weight loss. Ghrelin, known as the "hunger hormone," is produced in the stomach. Ghrelin levels decrease after sleeve gastrectomy, leading to a reduction in hunger and cravings.
While sleeve gastrectomy is considered less invasive and has a lower risk of complications compared to other weight loss surgeries, such as gastric bypass, it is still a major surgery and should be approached cautiously. As with any surgery, there are risks such as bleeding, infection, and blood clots.
It is important to note that weight loss surgery should be considered as a last resort after all other options have been exhausted. Patients should also be under the close supervision of a medical professional and have a comprehensive evaluation before surgery to ensure they are appropriate candidates. Additionally, patients must make significant lifestyle changes, including regular exercise, healthy eating, and follow-up with their medical team to ensure the best outcome.
Frequently Asked Questions (FAQs)
A: Also known as metabolic surgery or weight loss surgery, encompasses a variety of procedures designed to help individuals achieve significant and lasting weight loss.
These procedures work by altering the digestive system, either by restricting the amount of food the stomach can hold or by bypassing a portion of the digestive tract to reduce calorie absorption.
A: This procedure is typically recommended for individuals who:
- Have a Body Mass Index (BMI) of 40 or higher, or a BMI of 35 or higher with obesity-related health conditions such as type 2 diabetes, high blood pressure, or sleep apnea.
- Have tried and failed to lose weight through traditional methods like diet and exercise.
- Are committed to making long-term lifestyle changes, including following a healthy diet and engaging in regular physical activity.
- Are in good overall health and able to undergo surgery.
A: Kamol Hospital offers several types of bariatric surgery, including:
- Gastric Sleeve Surgery: This procedure removes a portion of the stomach, creating a smaller, sleeve-shaped stomach. This restricts the amount of food you can eat and helps you feel full faster.
- Gastric Bypass Surgery: This procedure creates a small pouch at the top of the stomach and connects it directly to the small intestine, bypassing a portion of the digestive tract. This reduces the amount of food you can eat and limits calorie absorption.
- Adjustable Gastric Banding: This procedure involves placing an adjustable band around the upper part of the stomach, creating a small pouch. The band can be adjusted to control the amount of food that can pass through.
A: The procedure can lead to significant weight loss and improve or resolve obesity-related health conditions, such as:
- Type 2 diabetes
- High blood pressure
- High cholesterol
- Sleep apnea
- Joint pain
- Infertility
It can also improve your overall quality of life, increase energy levels, and boost self-esteem.
A: As with any surgical procedure, weight loss surgery carries potential risks and complications, including:
- Bleeding
- Infection
- Blood clots
- Leaks from the surgical site
- Nutritional deficiencies
- Dumping syndrome (a group of symptoms that can occur after eating, such as nausea, vomiting, and diarrhea)
These complications are rare, and our experienced surgeons take every precaution to minimize risks.
A:Metabolic and bariatric surgeries are often related but serve different purposes in addressing weight and metabolic disorders:
-
Bariatric Surgery
Purpose: Specifically designed for weight loss in individuals with severe obesity.
Examples: Gastric bypass, sleeve gastrectomy, and adjustable gastric banding.
Focus: Alters the stomach and/or digestive tract to limit food intake or absorption.
Candidates: Primarily for individuals with a high Body Mass Index (BMI), usually over 40 or 35 with obesity-related conditions.
-
Metabolic Surgery
Purpose: Targets metabolic disorders, such as Type 2 diabetes or insulin resistance, and weight loss may be a secondary benefit.
Examples: Similar procedures to bariatric surgery (e.g., gastric bypass), but the intent is to treat metabolic disease.
Focus: Improves or resolves metabolic conditions through hormonal and metabolic changes, not solely weight reduction.
Candidates: Those with metabolic conditions, even with a BMI lower than traditional bariatric criteria.
In summary, while both types of surgeries involve similar procedures, the primary goals differ—bariatric surgery focuses on obesity and weight loss, whereas metabolic surgery targets underlying metabolic diseases.
A: The amount of weight you lose after metabolic / bariatric surgery depends on the type of surgery you have, your commitment to positive lifestyle changes, and a number of individual factors.
Most people lose a significant amount of weight within the first year after surgery.
A: Yes, you will need to follow a special diet after weight loss surgery. This diet will be tailored to your individual needs and the type of surgery you have. It will typically involve eating smaller, more frequent meals, focusing on protein and nutrient-rich foods, and avoiding sugary drinks and high-fat foods.
A: You may need to take certain supplements after bariatric surgery to prevent nutritional deficiencies. This is because your body may not be able to absorb all the nutrients it needs from food after the surgery.
Your surgeon and a registered dietitian will work with you to determine which supplements you need.
A: The length of your hospital stay will depend on the type of surgery you have and your individual recovery. Most people stay in the hospital for 1-3 days after surgery.
A: You can expect some pain and discomfort after weight loss surgery. This can be managed with pain medication. You will need to gradually increase your activity level and follow a special diet as you recover. Most people can return to work and normal activities within a few weeks.
A: Yes, you will have scars after Metabolic / bariatric surgery. However, the incisions are typically small and placed in discreet locations. The scars will fade over time.
A: The cost of weight loss surgery can vary a fair bit, depending on the type of surgery you have and various individual factors.
We offer competitive prices and transparent pricing policies. Please feel free to contact our hospital directly for a personalized quote and to discuss financing options.
A: Insurance coverage for this procedure varies depending on your specific insurance plan. It's important to check with your insurance provider first to determine your coverage.
A: Your surgeon will provide detailed instructions on how to prepare for your surgery. This may include:
- Undergoing a pre-operative medical evaluation.
- Losing a certain amount of weight before surgery.
- Stopping certain medications or supplements.
- Quitting smoking.
- Attending pre-operative counseling sessions.
A: If you have a burning question that isn’t covered here, please do not hesitate to get in touch with the team at Kamol Hospital directly with any further questions you may have.
Our friendly and knowledgeable staff are available to provide you with the information and support you need to make a well-informed decision.